Reinjury rates after ACL reconstruction are 20% for those that return to sport, 23% for those under age 25 who return to sport per Wiggins, and 5% for professional athletes who meet discharge criteria and return to sport, according to Grindem. If someone requires ACL revision surgery due to re-injury, there is a 30% failure rate, and additional physical therapy is necessary. In light of these statistics, we need to have criteria to determine the most appropriate time to return to sport to minimize re-injury rates.
Evidence supports that post-operative timelines are not the best determination for return to sport. Research shows waiting nine to 12 months and over 12 months for those under age 20 decreases re-injury risk after ACL reconstruction. Grindem has demonstrated that re-injury is further reduced to 3.5% to 5% by waiting nine months to return to sport and passing testing criteria. Capin et al. reported in 2019 in BJSM that passing a return to sport test battery is associated with decreased chances of an ACL injury by 75% and ACL graft rupture by 78%.

Manske reports that testing needs to be comprehensive using a battery of tests, as compensation can hide deficits during functional movement. Using only the opposite leg for comparison can also deceive decisions of when to return to sport, as research shows the contralateral limb has a decline in strength and power during the recovery process. My colleague, Leo Quinn, PT, and I have seen this repeatedly when testing our post-op ACL patients who can relatively quickly match their opposite limb measurements, but they are still not functional.
As reported in Part 1 of this series, at Rose City Physical Therapy, we use the BodiTrak pressure mat for clinical decision-making for our patients’ treatment progression. And for the athlete, it is used as an objective evaluation tool for return-to-sport decision-making through data capture and achieving goals established by research. In ideal cases, we try to measure these metrics before surgery to provide data to compare to testing and training after surgery. We evaluate squatting, hopping, and jumping variations. For any deficits, we rehab to decrease injury risk patterns, increase performance, and reduce future injuries. Evidence shows that faulty landing mechanics from a jump may indicate injury risk.
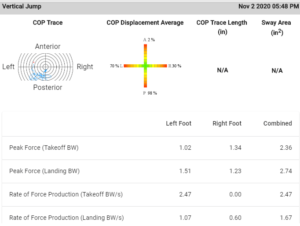
We know from research that only putting in the physical therapy work as an athlete is not enough. We need measurements that provide metrics that are not visible without sensors and technology to provide data analysis and outcomes. Some of the recommended metrics are the Rate of Force Development (RFD), Dynamic Vertical Force (DVF), Ground Reaction Force (GRF), and Reactive Strength Index (RSI).
- RFD is a measure of the power of how quickly you can generate force
- DVF is relative to the force of a person’s body weight
- GRF is the magnitude of force generated on a surface
- RSI is the strength and dynamic, explosive power index. It demonstrates the athletes’ ability to rapidly change from eccentric to concentric contractions during the stretch-shortening-cycles in jumps such as the incremental drop jump, countermovement jump, and squat jump. It reflects a healthy relationship for directional change speed, acceleration speed, and offensive and defensive agility. This metric is best measured once the athlete has achieved technical proficiency with plyometric movements. The RSI can also be used to calculate the Dynamic Strength Index, which is the difference between an athlete’s maximal and explosive strength capacity, which helps guide whether an athlete needs to focus on maximal strength or Rate of Force Development.
These metrics give a detailed objective picture of the athlete’s current athletic function and performance. An athlete can compensate and offload, or alter loading, on the surgical leg. This asymmetry can continue with single-leg squat, hopping, jumping, and running – unless discovered and corrected. And if not corrected, compensations can lead to re-injury, other injuries, and decreased performance. We can measure jump distance or height without BodiTrak, but we would not know if the athlete has a slower RFD, which research is finding is linked to the athlete’s perception of outcome. Anecdotally, I see the data match up with the psychological confidence of jumping, landing, and cutting.
In 2012, Angelozzi in JOSPT showed that professional soccer players who underwent ACL reconstruction achieved strength within six months but RFD not until 12 months. Argemi, in BJSM in 2017, reports that RFD is a factor for post-op ACL patients, as well as other lower extremity injuries, and force plate measurements indicate a patient’s functional level during physical therapy and help to determine parameters to a full return to sport.
With all the effort put into post-operative physical therapy through treatment progressions, reassessment, modification, and the patient’s clinic and home exercises, the same attention and focus is necessary with return-to-sport decisions. Objective data and metric-based performance indicators assure optimal rehabilitation and inform the readiness for return to sport and beyond.
The 2016 Consensus Statement on Return to Sport explains the continuum of return to participation, return to sport, and return to performance, showing that assessment, rehab, and training continue beyond returning to the field. The determination to return to sport is not the endpoint as at that point, as the athlete will not be at their peak performance. Training continues to increase performance and decrease injury. Bergtsson et al. in 2019, BJSM reported that athletes who completed less than four practice sessions before returning to competition had a three times higher injury risk. With each additional training session, injury risk decreased by 7%, and a minimum of six sessions is recommended before returning to competition. Also, in BJSM, Blanch and Gabbett, in 2016, report a strong predictive value between acute:chronic workload ratio and injury likelihood to help determine if an athlete has trained enough to assist in the return to sport decision. No longer is the timeline a determination for post-operative return to sport and performance. If you need training with the BodiTrak Pressure Mat, contact our office in Portland, OR today!